News & stories, First In Canada with Illumisite
May 2023
Saint John Thoracics team performs first in Canada fluoroscopic navigation bronchoscopy.
Imagine you set out on a road trip and you're not sure where you’re going—what do you do? Plug the address into your GPS to guide you to your destination, right?
Illumsite technology is like a GPS for surgeons. It helps surgeons find and treat abnormal lung tissue—also called nodules—more effectively by directing them with precision and accuracy.

“When you plug an address into your GPS it maps a route,” says Dr. Brian Johnston. “Your GPS takes you through the roads and turns to get to your destination. The Illumisite platform essentially does the same thing.”
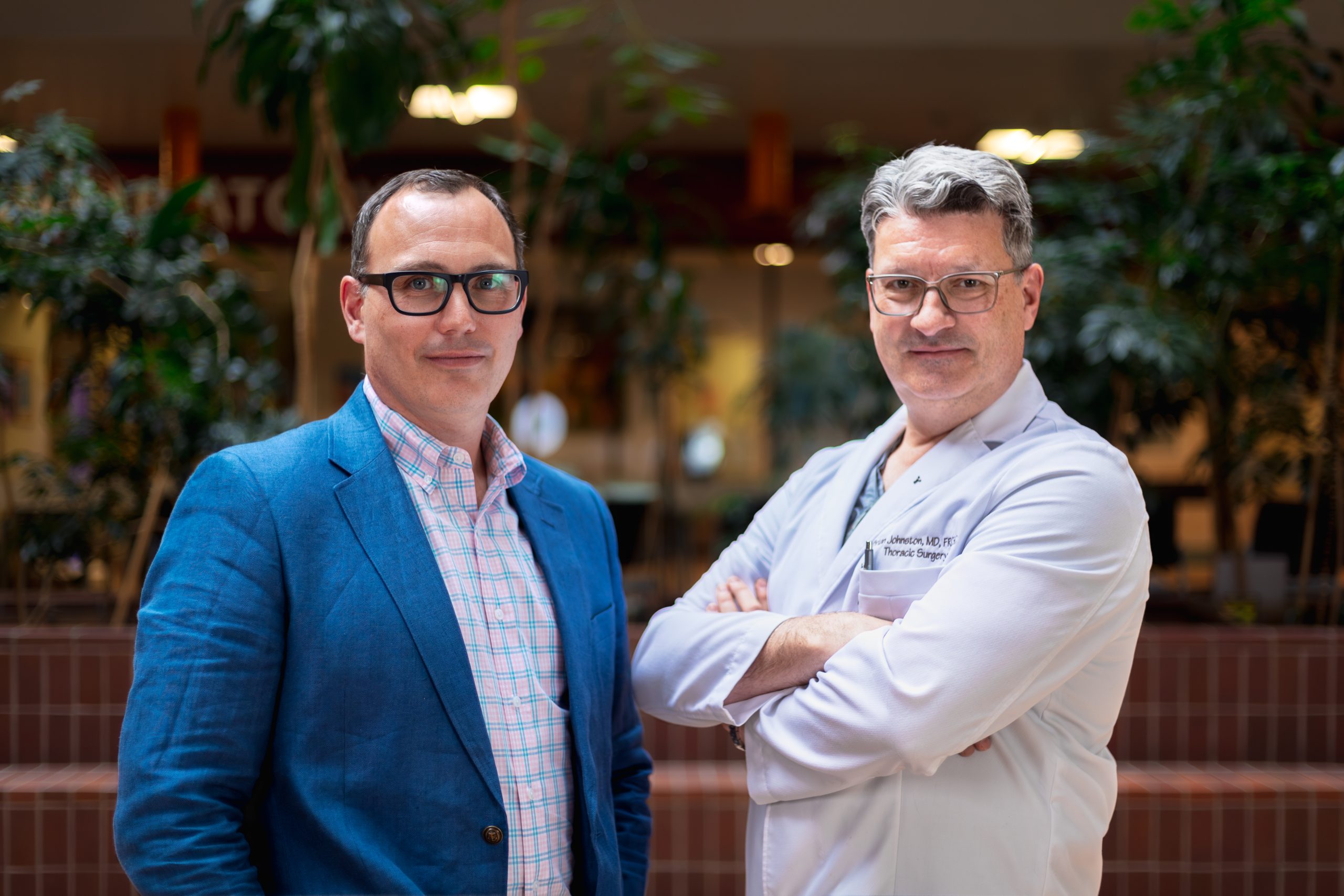
Dr. Brian Johnston and Dr. Crispin Russell are both thoracic surgeons at Horizon’s Saint John Regional Hospital, and recently performed the very first fluoroscopic navigation bronchoscopy procedure in Canada using Illumisite.
What is fluoroscopic navigation bronchoscopy?
Fluoroscopic navigation technology is a minimally invasive procedure that allows clinicians to access difficult-to-reach abnormal lung tissue with greater accuracy. It uses GPS-like technology to guide endoscopic tools, making it possible to reach areas not accessible with traditional bronchoscopy.
Illumisite uploads information from a lung patient’s CT scan and provides real-time imaging that takes into account the difference between the static CT scan and the dynamic breathing lung. Illumisite corrects for CT-to-body discrepancies and enhances the visibility of the abnormal tissue. It also allows physicians to guide endoscopic tools or catheters in the pulmonary tract and to place radiosurgical and dye markers into soft lung tissue to guide thoracic surgery.
“We do a real time X-ray called fluoroscopy to more accurately locate the nodule and then we're able to reach more distal nodules using the special catheters that are associated with the system with greater accuracy, using the CT scan and the and the real time X-ray,” says Dr. Russell.
The tool allows them, on the day of the procedure, to travel with greater accuracy—within a centimeter or less to the nodule—so they can biopsy and potentially treat nodules.
First cases prove successful
The first cases using the Illumisite technology went exceptionally well. “All the procedures that we've done to date have been successful in giving us the information that we need to make clinical decisions,” says Dr. Johnston. Medtronic, the company which provided the training, was also on site for the first case to assist.
“They coordinated training for all the other members of the team, including X-ray nursing cytology the day before we did our first procedures so it made everything go very smoothly.”
Because of the success, the team is already planning more procedures.
“We’re planning to do four a month to start,” says Dr. Johnston, “and we will see how things go and grow from there.”
Having Illumisite has already proved its worth, with the team successfully obtaining tissue samples to inform clinical decisions. For example, it allows the clinicians to collect enough samples until the lab team advises that they have adequate tissue to make a diagnosis.
“Prior to Illumisite, a patient could come in for the traditional procedure, and if we weren’t successful in getting a good specimen, then they may need to come back a couple more times or we might need to have a different procedure done,” says Johnston. “So it’s a real benefit.”
Among benefits are mitigated risk to patients, as well as more accurate care
Because this procedure is minimally invasive and more accurate, it means patients can recover faster and get back to their lives with less disruption.
“Traditionally if we found a suspicious lung lesion, one of the most accurate ways to get tissue diagnosis was what’s called a transthoracic needle biopsy,” says Dr. Russell.
“Patients would have to go to the X-ray Department, be sedated, frozen, and then physicians would put a needle through the skin into the chest and through the lung into the lesion.”
With all those factors, the logistics required to perform the procedure are complicated. And that can lead to long wait times from the time of the initial consultation to the time of the procedure.
A collapsed lung occurs when air escapes from the lung. The air then fills the space outside of the lung between the lung and chest wall. This buildup of air puts pressure on the lung, so it cannot expand as much as it normally does when you take a breath. The medical name of this condition is pneumothorax.
In addition, Dr. Russell points to the fact that there is also a risk of pneumothorax, or a collapsed lung.
“The risk of pneumothorax with a transthoracic needle biopsy is between 10 and 20%,” says Dr. Russell. “Requiring a chest tube and hospital admission. Those are real time risks.” With Illumisite, the risk drops significantly.
“One of the biggest advantages is that with Illuminisite, the risk of pneumothorax is reduced to about 3% versus 10 to 20% with a traditional procedure. So it’s an outpatient procedure.”
Ability to attract and retain new talent and develop the program
In addition to the patient benefits, there are also implications for attracting new talent.

“New graduates from surgical training programs want to come to centres where there's the most up-to-date and current techniques available. So this will dramatically help from a recruitment point of view, and hopefully retention,” says Dr. Johnston.
Being able to access this type of technology, thanks to the generosity of donors, is something that Dr. Johnston feels would be attractive to medical students.
“It’s encouraging that we have donors who are willing to help provide these technologies. A medical student could look at that and know they would be able to count on support in the future for endeavors that might come to light in the next few years. It’s encouraging.”
It’s a huge step forward in treatment of lung cancer patients, and with it being more minimally invasive, “we can get the patient home faster and back to work faster or back to whatever quality of life they had previously.
- Dr. Russell
That forward thinking and growth is something that Dr. Russell sees as a real benefit and focus of the program as well.
“Not just looking at what we can do with it now, but looking at what we can do with it in the future,” says Dr. Russell.
Ultimately, the hope would be to treat the lung cancers the same day patients come for the diagnostic procedure with the ability to potentially mark the procedures if they do need an operation
Leading-edge technology is a breath of fresh air for lung cancer care clinicians
One of the challenges in providing care to lung cancer patients is the stigma around lung cancer.
“The fact remains that lung cancer, you know, continues to have a stigma attached to it,” says Dr. Johnston.
According to StatisticsCanada, lung cancer is the leading cause of cancer deaths at 25%, with colorectal cancer at 11% and pancreatic cancer at 7%.
“And so it doesn't receive the same funding from research and for clinical care as as other types of cancers do,” Dr. Johnson continues, “despite the fact that it's the most deadly cancer.”
Outside of the stigma, there was also the factor of size. Given the size of the department at the Regional, the state-of-the-art technology is a great addition, but also an achievement.
“Although we're a relatively small thoracic surgery centre and despite our lower population and hospital size we're able to provide the most up to date and current care,” says Dr. Johnston.
For those reasons and more, Dr. Johnston says it’s “a significant feather in the cap to the community, the donors and the hospital to be able to achieve that.”
Support for the technology was thanks to donors
The Illumisite technology was acquired through funding secured as part of the hospital foundation’s last medical competition, Lion’s Den.
“Having the Illumisite technology here at the Regional wouldn’t have been possible without the donors and the foundation,” says Dr. Johnston. “If we didn't have this support, we wouldn't be performing the advanced procedures and growing the scope of the work that we do,” says Dr. Johnston.
Both Dr. Johnston and Dr. Russell were part of Team Enhanced Lung Cancer Care, who pitched for leading-edge diagnostic equipment for earlier detection and treatment.
“I’d like to express my sincere thanks and gratitude to the foundation and all the donors whose generous support has really allowed us to make this happen. You took a dream and made it reality and we can’t thank you enough,” says Dr. Russell.


